Welcome to my blog ‘What Causes Dysbiosis’.
In this blog you will gain a better understanding of what dysbiossis is, what causes dysbiosis, and how to fix dysbiosis. Many will know that various medications such as antibiotics and a poor diet can cause it, but not as many may appreciate that our own cells have a key role to play within maintaining a healthy microbiome and when cell function is compromised, dysbiosis will develop. The cells in question are the colonocytes – read on to understand this essential gut health topic.
What Is Dysbiosis?
The most typical features of dysbiosis are:
- A decrease in the diversity of bacteria.
- A loss of beneficial bacteria.
- An overgrowth of potentially harmful bacteria. (source)
You might be surprised to know there isn’t a more comprehensive definition of dysbiosis that is universally accepted. It is near on an impossible task to define both what a healthy microbiome looks like, and what an unhealthy microbiome looks like. This is because the gut microbiome is a highly diverse ecosystem that differs between individuals, and shifts with changes in the diet and lifestyle.
For example, the microbiome should ideally change throughout the seasons as different foods become more, or less, readily available. We are entering a phase in time when our physiology is experiencing less and less fluctuation, less ebb and flow as it becomes less and less connected with nature.
However when you scour the research there is definitely a theme that emerges. And that is a bloom (overgrowth) of proteobacteria, also referred to facultative bacteria. This was the conclusion of one paper:
Perhaps the most consistent and robust ecological pattern observed during gut dysbiosis is an expansion of facultative anaerobic bacteria belonging to the phylum Proteobacteria.
A quick definition will be helpful here…
Obligate anaerobes (these make up the vast majority of the microbiome) are bacteria that can only grow and reproduce in an environment largely devoid of oxygen. They also include bacteria that produce short chain fatty acids such as butyrate (much more on this later).
Facultative anaerobes which make up a tiny percentage of the microbiome are capable of growing and reproducing in an environment with or without oxygen. Facultative anaerobes include many gut pathogens.
Now we know more about what dysbiosis is, let’s explore the question what causes dysbisois?
Gut Dysbiosis Symptoms
Dysbiosis has been associated to many chronic human illnesses, including obesity, colorectal cancer, diabetes, arthritis, asthma, cardiovascular disease and neurological disorders.
Gastrointestinal symptoms include bloating, diarrhoea, constipation, food sensitivities, and abdominal pain but sometimes symptoms only manifest outside of the gut and might include brain fog, fatigue, or one of the aforementioned conditions.
Testing For Dysbiosis
You can test for dysbiosis via an at-home gut microbiome test.
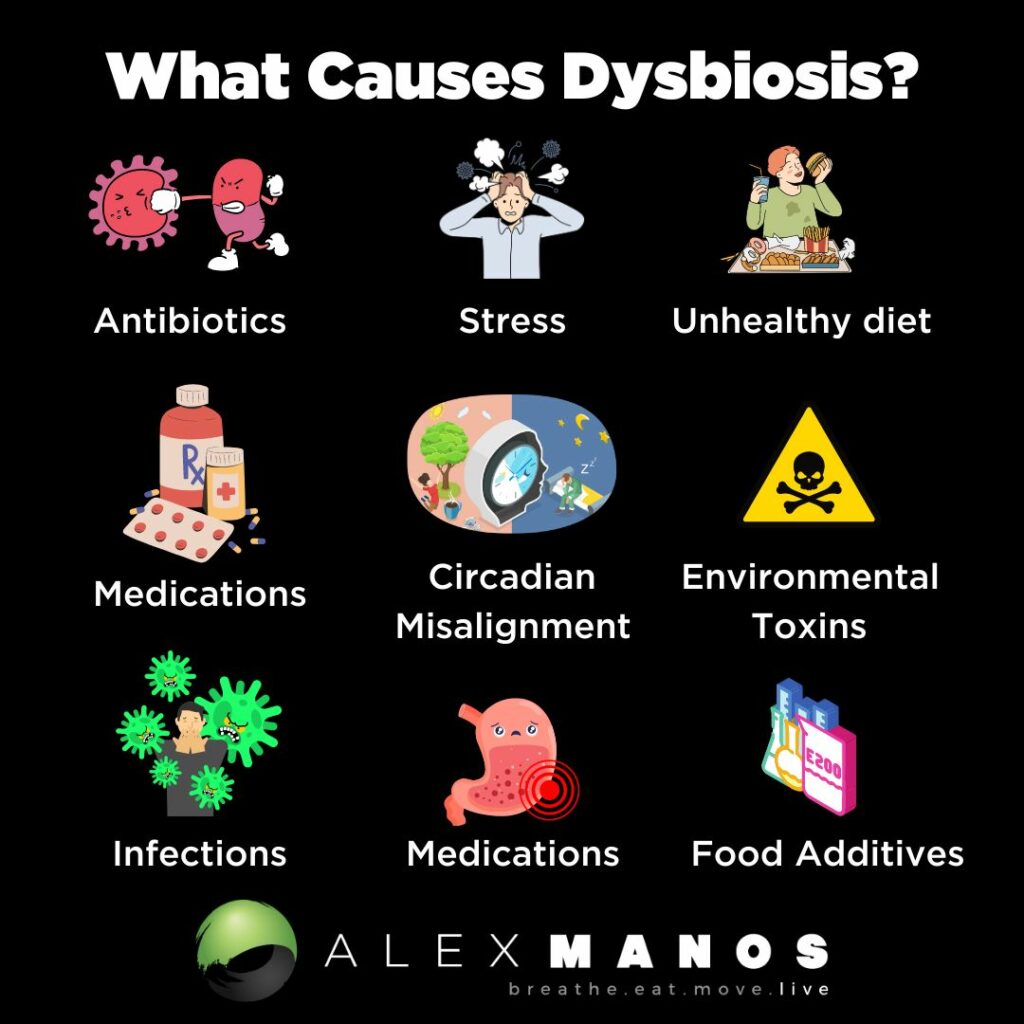
What Causes Dysbiosis?
There are various factors, both internal and external, that cause dysbiosis.
Food Additives
The effect of food additives on the gut microbiome has long been overlooked, but recently, several groups, have published data showing that some gut bacteria are very sensitive to preservatives and, also, that exposure to common food preservatives promotes overgrowth of proteobacteria. Other categories of additives have also been shown to have negative effects on human health. For example, dietary emulsifiers directly alter the composition of the human gut microbiome and trigger inflammation. (source)
Smoking
In human microbiome studies, tobacco smokers displayed a higher relative abundance of Prevotella, lower relative abundance of Bacteroides, and lower gut microbiome diversity compared to controls. Interestingly, smoking cessation induced profound changes in the gut microbiome, including an increase in microbiome diversity, an increase of Firmicutes and Actinobacteria, and a decrease in Proteobacteria.
Most importantly, the composition of the gut microbiome of smokers and non-smokers were different when fed identical meals to avoid the influences of dietary factors (source).
Sedentary Living
Research has found that professional rugby players, have greater microbiome diversity, compared to lean sedentary people, with a higher relative abundance of 40 different bacterial taxa. Research has also found that women who performed at least 3 hours of exercise per week had a greater abundance of Faecalibacterium prausnizii, Roseburia hominis, and Akkermansia muciniphilia compared to sedentary controls – these are referred to as key stone species as they are known to have a particularly prominent role in gut health. Akkermansia has been associated with lower body mass index and improved metabolic health, and Faecalibacterium prausnitzii and Roseburia hominis both produce the short chain fatty acid butyrate.
Overall, there is strong evidence that exercise can benefit the gut microbiome by improving microbiome diversity and increasing butyrate production (source). As we will see later, butyrate is essential in maintaining healthy colonocyte metabolism which is essential in maintaining a healthy microbiome.
Environmental Toxins
Research on the toxicity of environmental toxins in gut microbiome has gained prominence in recent years. Various factors, such as air pollution, chemicals, heavy metals, and pesticides, have a detrimental impact on the composition and functioning of the gut microbiome (source).
Circadian Misalignment
Another factor as to what causes dysbiosis us poor sleep habits.
Insufficient sleep alters the microbiota with potential implications for dysregulated metabolism.
Findings from initial controlled laboratory studies of insufficient sleep and changes in the human gut microbiome community structure have been inconsistent. Specifically, two days with 4.25h sleep opportunities and five days with 4h sleep opportunities did not alter beta diversity; whereas two days with 4.25h sleep opportunities increased the F:B ratio and increased relative abundance of families Coriobacteriaceae and Erysipelotrichaceae and decreased Tenericutes in one of the studies (source)
A New Understanding Of Dysbiosis
Gut dysbiosis is secondary to impaired mitochondrial disturbance
The above quote comes from this paper, which explored the role of butyrate in “fine tuning” colonic homeostasis.
So many of us know the above, commonly cited, causes of dysbiosis such as poor dietary choices and antibiotics.
What many people don’t know is that our own cells, in particular colonocytes (cells that line our colon), have a profound impact on the microbiome.
“The energy metabolism of colonic epithelial cells functions as a control switch of the gut microbiota, mediating shifts between homeostatic and dysbiotic communities.” (source)
A critical thing to understand is that the immune system maintains homeostasis by shaping the microbiome to be helpful. The microbiome does this via numerous ways but one of them is to aid in the digestion of nutrients that cannot be processed by our own digestive enzymes. Specifically, complex dietary carbohydrates (fiber) are broken down by the gut bacteria into fermentation products that are absorbed and contribute to our immune development among many other things.
We all hear about the importance of microbiome diversity and this is one of those reasons – bacterial diversity increases the probability of including species of bacteria that can break down complex carbohydrates and produce short chain fatty acids like butyrate.
However, facultative anaerobic bacteria (remember we mentioned these at the beginning -they are capable of growing and reproducing in an environment with or without oxygen), such as Proteobacteria, do not specialise in fermenting fiber. So, viewing our ‘control’ over the our gut microbiome from an ecological perspective predicts that “our immune system maintains homeostasis by shaping the colonic microbiota to be diverse and dominated by obligate anaerobic bacteria, thereby ensuring this microbial community provides benefit by generating fermentation products from fiber”. (source)
Research shows that colonocytes (cells that line the colon) play a central role in this process.
PPARγ activates fatty acid metabolism, resulting in mitochondrial β-oxidation of long-chain and short-chain fatty acids and oxygen consumption through oxidative phosphorylation. (source)
Since oxygen freely diffuses across biological membranes, epithelial hypoxia limits the amount of oxygen emanating from the mucosal surface, which helps maintain anaerobiosis in the intestinal lumen. In turn, anaerobiosis ensures the colonic microbiota is dominated by obligate anaerobic bacteria, which provide benefit to the host by converting fiber into fermentation products. Through this mechanism, the colonic epithelium shapes the microbiota to be beneficial, thereby maintaining gut homeostasis. (source)
We now know that the population of facultative anaerobic bacteria expands in the colon during dysbiosis because a disruption of epithelial hypoxia increases the amount of oxygen emanating from the gut lining.
Thus, the shift in the colonic microbiota composition from obligate to facultative anaerobic bacteria, associated with many chronic human illnesses, might have a common underpinning in colonocyte dysfunction.
The Role Of Butyrate
Butyrate activates PPARγ signaling to drive the metabolism of surface colonocytes towards mitochondrial β-oxidation of fatty acids, which is important for maintaining epithelial hypoxia.
Antibiotics lead to a depletion of bacteria that produce short-chain fatty acids such as butyrate, and this causes a down regulation in PPARγ signaling.
This shifts the metabolism of colonocytes towards anaerobic glycolysis, one which uses little oxygen This results in a an increase in oxygen levels which, in turn, increases the amount of oxygen emanating from the mucosal surface, thereby driving an expansion of facultative anaerobic bacteria by aerobic respiration.
So a key consideration to the question “what causes dysbiosis” is butyrate, or a lack of more specifically. We can test for butyrate producing bacteria via stool testing.
Is Dysbiosis The Same As Leaky Gut?
Dysbiosis is not the same as leaky gut, but they can be related.
Dysbiosis refers to an imbalance in the microbiota, where as leaky gut refers to intestinal hyper permeability – the lining of the gut has become more permeable than it should be. You see the the gut lining is ‘selectively permeable’ meaning it allows somethings through, such as nutrients, but doesn’t allow other things through, such as bacteria.
For various reasons, including dysbiosis, the lining of the gut can become more permeable (i.e leaky) and thus things get through that shouldn’t. This results in an inflammatory response from immune cells.
Listen to my interview with Dr. Jenna Macciochi on leaky gut and inflammation here.
How To Fix Dysbiosis
My Interview with Kiran Krishnan
Now we understand what causes dysbiosis, the interventions to fix it become more obvious. Kiran does a great job of summarising some of these in the above video.
Dietary Diversity
There is a correlation between how diverse your diet is, and how diverse your gut microbiome is. So a simple strategy to support a healthy microbiome is to eat a diverse diet. Focus on eating as many local in season foods as you can.
Prebiotics
Prebiotics can be found in our diet and good sources include leeks, onion, garlic, asparagus, wheat and legumes. But we can also consider supplementing prebiotics. One common recommendation is PHGG, partially hydrolysed guar gum.
Intake of PHGG for three months has been shown to significantly improve stool form, evaluated using the Bristol Stool Scale. Stool testing detected significant changes in the ratio of some bacteria, such as an increase of Bifidobacterium also.
Recommended Product: PHGG.
Polyphenols
Polyphenols are what give food their colour so eating a diet that is colourful will ensure a high intake of polyphenols. Good options include green tea, coffee, dark chocolate, olives, olive oil, tomatoes, peppers, berries, grapes (the list goes on!).
Recommend Product: Bio.Me Essential
Probiotics
As always it is important to take a food first approach and thus we can consider incorporating fermented produce in to the diet as a way to get live bacteria in the our guts. Kefir, sauerkraut, kimchi and live yoghurt are all good options.
In regards to probiotic supplementation, arguably this needs to be tailored to the individual. Specific probiotic strains can be selected for specific reasons, for example some probiotics have been shown to be helpful for diarrhoea such as saccharomyces boulardii or lactobacillus rhamnosus GG, while others have evidence behind them for constipation or anxiety.
Postbiotics
We now have a sound understanding how butyrate helps maintain a healthy microbiome via its role on PPAR and colonocyte metabolism. Butyrate is a post biotic – which essentially is something produced by our gut bacteria. We can support butyrate production via consuming adequate amounts of dietary fibre, especially resistant starch. A nice little hack is to regularly eat cooked and cooled potatoes or rice which contains high amount of resistant starch. So a practical example would be having something like a potato salad as part of a meal. As we’re about to see another way to support butyrate is to stay physically active.
Exercise
Exercise improves both the diversity of the gut microbiome and the function of the microbiome. Research has shown that regular exercise supports butyrate production – butyrate has an essential role to play within gut health as it is a fuel for the colonocytes that line the gut. But it also has anti-inflammatory, pro-motility and antimicrobial properties. A systematic review published in 2023 concluded:
“The findings show that participation in exercise of moderate to high-intensity for 30–90 min ≥3 times per week (or between 150–270 min per week) for ≥8 weeks is likely to produce changes in the gut microbiota. Exercise appears to be effective in modifying the gut microbiota in both clinical and healthy populations. “
Stress Management
We can not overestimate the impact chronic stress has on our digestive systems. In fact a 2020 study demonstrated that mindfulness-based stress reduction training was associated with robust improvements in gut symptoms. There were significant increases in three of the five measured facets of mindfulness, but regression analyses suggested that increases in the ability to retain present moment focus and act with awareness were particularly important for improving outcomes in those with IBS (source).
Alex is a certified Functional Medicine Practitioner (IFMCP) and has a MSc in Personalised Nutrition. He is also a breathwork facilitator with a background in personal training and massage therapy. He also runs The Resiliency Program - a 24 week program aimed at building physical, mental, emotional, and spiritual resilience.