What Is Brain Fog?
Brain fog isn’t actually a medical condition in its own right, and there are no diagnostic criteria. It is similar to conditions such as irritable bowel syndrome or chronic fatigue syndrome – it is an umbrella term that covers a range of symptoms associated with poor cognition (source).
Symptoms may include:
- Slowness of thought.
- Trouble focusing and maintaining concentration.
- Issues with forgetfulness
- A general haziness in thought processes.
(source)
It is very real and can be very debilitating. I worked with one client who had to retire from her teaching career due to the extent of her brain fog.
“From a viral or treatment consequence that has traditionally received, at best, modest levels of attention, long Covid has forced the conversation around brain fog onto centre stage.”
Today, there are dozens of conditions that are associated with brain fog, including conditions associated with histamine, such as allergies and MCAS, menopause, ADHD, and even kidney failure, as well as conditions such as anxiety and depression.
Let’s dive into some of the known causes.
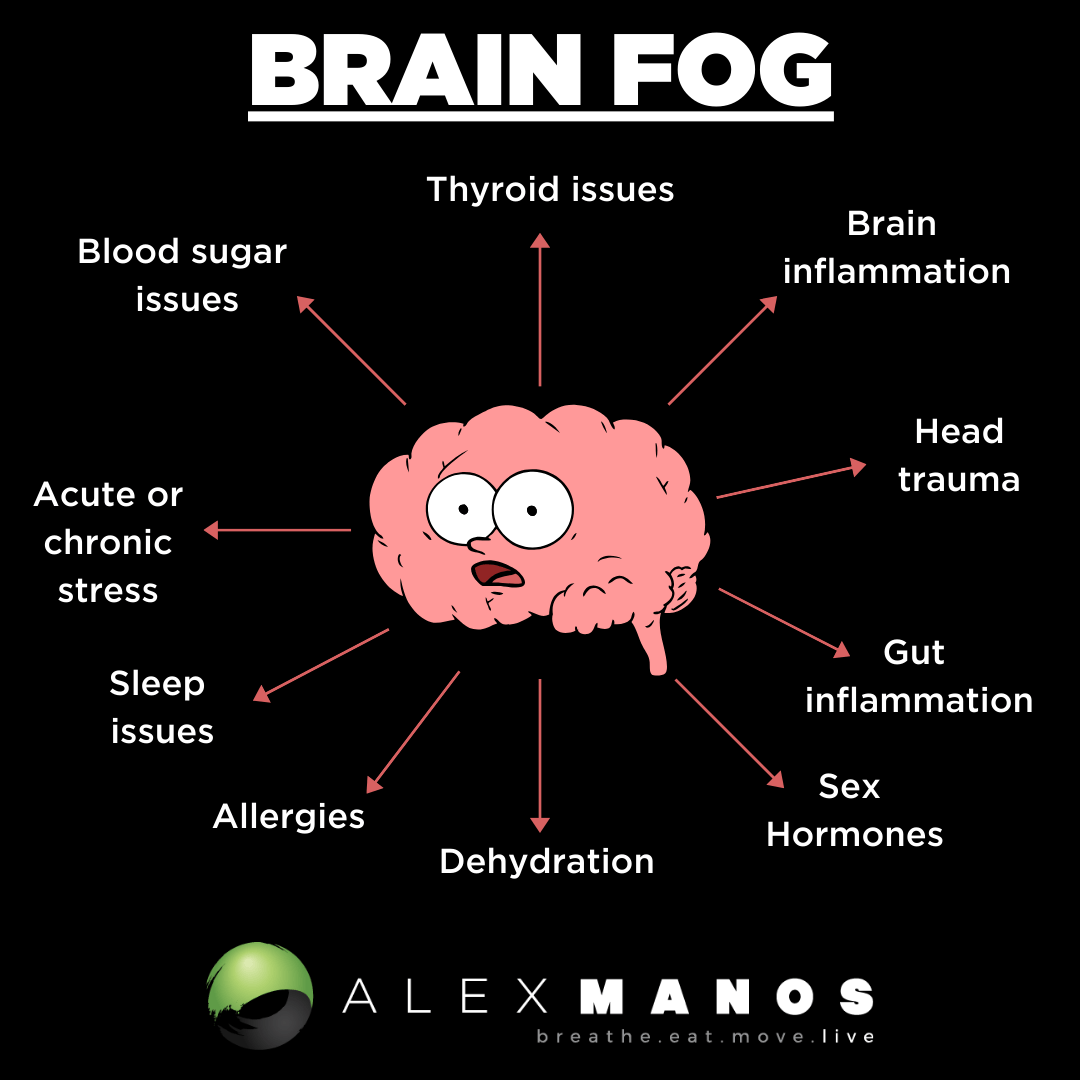
What Causes Brain Fog?
- Brain inflammation.
- Chronic stress.
- Thyroid issues.
- Dehydration and electrolyte imbalances.
- Blood sugar dysregulation.
- Gut inflammation.
- Food sensitivities.
- Sex hormone issues.
- Sleep issues.
- Head Trauma.
Brain Inflammation
I want to start with brain inflammation because if we have a basic understanding of brain inflammation and how the immune system is involved, we’ll instantly understand how things like blood sugar dysregulation, gut inflammation, or stress can cause brain fog.
To understand brain inflammation, we need to understand a little about microglia in the brain.
What Are Microglia?
Microglia are resident cells in the brain and are found throughout the central nervous system.
These cells are critical in the way in which our bodies react to an immune system challenge.
They regulate brain development, maintenance of neural networks, and injury repair.
They are constantly assessing their environment, and when the body comes under attack from possible sources of infection, the glial cells act as the first responders.
As part of this response is the release of proinflammatory cytokines (inflammatory molecules produced by certain immune cells), thus creating an inflammatory signalling process. The resultant inflammation is usually short-lived, lasting long enough to deal with the immune system challenge.
The problem arises when they become chronically hyperactive.
When the activation of microglia becomes impaired, it can lead to inflammation.
Sustained activation of microglia is likely to play a pivotal role in the chronic neuroinflammation and chronic symptoms following on from SARS-CoV-2 infection.
Inflammation in the brain, caused by this heightened immune reaction, negatively impacts neural networks, which leads to cell damage and death. The result is brain cells that find it harder to send signals to each other and a brain that struggles to complete its normal tasks. An example of this would be making new neurons in the hippocampus – a part of the brain that has an important role in learning and memory. (source)
Inflammatory cytokines have been found to play a significant role in:
- Reductions in long-term potentiation (the sensitisation of nerve cells due to repeated synaptic excitation) and long-term depression (the process by which neurons become desensitised).
- A reduction in neurogenesis (the production of new brain cells).
- A reduction in dendritic sprouting (a reduction in growth of new branches in nerves)
(source)
As these functions play an integral role in brain plasticity, the ability of the brain to reshape its neural circuits, the individual’s ability to show cognitive flexibility is critically dependent on the body’s immune reactivity. (source)
You may be asking what causes brain inflammation; well, we could argue this blog post is partially answering that question too! Chronic stress, food sensitivities, infections, and head trauma, to name a few!
Chronic Stress
Not only do immune challenges such as infections prime glial cells, many things can, including chronic or acute stress.
“Excessive levels of anxiety can cause problems with how the brain functions and how it retains information. When anxiety monopolises the brain, other tasks suffer—including processing information, concentration, paying attention, and remembering. The result can feel like brain fog.” Dr. Amen.
3 tips to manage stress:
- Diaphragmatic breathing. Yes, it can be that simple – focusing on slowing the breath down and breathing deep into your belly is an evidence-based way to calm the mind and body. I recommend trying a breath rate or 5-6 breaths per minute (so a 5-second inhale and 5-second exhale).
- A mindfulness practice. Practising gratitude, meditating, yoga, tai chi, a walk in nature without distractions, and many other habits can be of great support here.
- Talk it out. Sometimes, we need to voice our concerns and share our challenges. Do not underestimate the power of a deep and meaningful conversation with a loved one.
Thyroid
Brain fog is frequently reported in patients with hypothyroidism, something that can easily be ruled in or ruled out with a simple blood test.
Interestingly, in the research, a small number of participants felt better when liothyronine (T3 medication) was added to their levothyroxine treatment (source).
Hydration And Electrolyte Status
Water accounts for 75% of brain mass, and research has discussed the fact that there may be associations between hydration and cognitive performance.
Next time you are feeling sub-par with your cognition – try adding a pinch of salt to some water and see if you notice a lift. It’s amazing how many people do!
Looking at this from the other perspective, dehydration has been shown to have negative effects on things such as short-term memory and attention. In one study, rehydration after water supplementation alleviated fatigue and improved short-term memory, attention, and reaction. (source)
Blood Sugar Dysregulation
Both high and low blood sugar levels can be harmful to the brain.
Diabetes is associated with poor cognitive function and changes in brain structure. People with both type 1 and type 2 diabetes have been shown to have mild to moderate reductions in cognitive function compared to healthy controls. (source)
One of the reasons behind this is that blood sugar fluctuations affect neurotransmitter levels.
Neurotransmitters are a large family of chemical messengers ( there are over one hundred known neurotransmitters). They regulate many physiological functions in both the central and peripheral nervous system.
They can be classified as either excitatory or inhibitory based on their function, and a healthy balance between these two categories of neurotransmitters is needed for a healthy brain. (source)
Researchers have reported that elevated blood sugar levels in type 2 diabetes, for example, dysregulate the excitatory-inhibitory balance between glutamate and GABA, causing cognitive impairment. (source)
In addition to the impact on neurotransmitters, fluctuating blood sugar leads to:
- Brain cell damage and degeneration
- Nerve damage
- Inflammation of the brain
- Injury to neurons due to insufficient glucose supply
(source)
Low blood sugar, which in my clinical practice is actually more common than high blood sugar, also needs to be considered.
Why?
Glucose is the brain’s fuel source. Balanced blood sugar levels are vital for a healthy brain chemistry and the prevention of neurodegeneration. When blood sugar is low, not enough glucose gets to the brain, and the brain will not be able to function optimally and will degenerate.
Anyone who has experienced a hypo, an episode of real low blood sugar levels, will know what this can feel like. You can feel spacey, light-headed, shaky, and irritable if they go too long without eating, and some simply won’t be able to keep their eyes open – their brains aren’t getting enough fuel to operate.
So hopefully, it is clear that balancing your blood sugar levels is one of the most important things to address when looking to improve brain health.
Chronic blood sugar imbalances are now suspected to contribute to the development of dementia and Alzheimer’s. In fact, some researchers are calling Alzheimer’s disease “Type 3 diabetes” due to the inflammatory blood sugar connection.
Symptoms of low blood sugar:
- Increased energy after meals
- Craving for sweets between meals
- Irritability if meals are missed
- Dependency on coffee and sugar for energy
- Becoming light-headed if meals are missed
- Eating to relieve fatigue
- Feeling shaky, jittery, or tremulous
- Feeling agitated and nervous
- Become upset easily
- Poor memory, forgetfulness
- Blurred vision
Gut Inflammation
“Brain fog has been extensively studied in patients with inflammatory bowel disease” (source)
Patients with IBD frequently complain of brain fog.
In one study, brain fog was correlated with systemic inflammation, although in this study, higher faecal calprotectin levels (a marker for inflammation in the large intestine) were unexpectedly associated with less cognitive impairment. (source)
Interestingly, the authors weren’t surprised by this, as they mentioned that they weren’t anticipating any relationship since systemic inflammation often doesn’t correlate with intestinal inflammation.
Having said that, experiments in mice have shown that inflammation in the colon results in an upregulation of inflammatory activity in the microglia of the hippocampus that, in turn, causes profound impairments in brain function (source).
In another paper, the authors discussed that the underlying mechanisms of this interaction (between the gut and brain) can be summarised as follows:
- Modulation of the gut barriers (i.e leaky gut).
- Modulation of afferent nerves.
- Production, expression, and turnover of neurotransmitters.
- Bacterial metabolites (such as LPS) and mucosal immune regulation.
(source)
Food Sensitivities
In one study, food allergy increased the number of microglia the percentage of active microglia, and induced inflammation in the cerebral cortex. Importantly, these changes were associated with behavioural impairments, including learning deficits. (source)
Ultimately, when there is an inflammatory response, microglia are going to be activated, hence brain fog.
Another obvious connection here is that brain fog is very common in histamine intolerance and mast cell activation. Histamine has been discussed as a potential trigger of brain fog (source) and will be released as part of the allergic response.
Sex hormone issues
“Neurological symptoms such as…brain fog…are a major complaint of women transitioning through menopause, with a significant impact on their quality of life, productivity and physical health.” (source)
Steroid hormones, which include the sex hormones that are active in the central nervous system, are called neurosteroids. They can be produced in the periphery (outside the central nervous system), where they are able to cross the blood-brain barrier, or synthesised in the central and peripheral nervous system by neurons and glial cells either from cholesterol or from local metabolism of intermediate hormones produced in the periphery.
Let’s just look at one sex hormone, oestrogen, to get a sense of how important they are in brain health and function.
Oestrogen hormones are connected to several neurotransmitter systems, including acetylcholine, serotonin, noradrenaline, and glutamate. In particular, the cholinergic neurotransmitter system is relevant in memory processes and, thus, brain fog.
Oestrogen exerts its positive action on the brain via neurotrophic (the growth of nervous tissue) and neuroprotective actions. For example, it enhances synaptic plasticity, neurite growth, and hippocampal neurogenesis and protects against neural injury.
Furthermore, oestrogen may improve mitochondrial function, enhancing energy production, which is super important when we consider the extremely high energy requirements of the brain.
Oestrogen also helps with DNA repair and promotion of antioxidant defences (source).
What’s key to understand here is that inflammation, mitochondrial dysfunction, and oxidative stress are all key factors in brain fog.
Sleep issues.
Sleep, along with diet and exercise, are all well known to help reduce inflammation in the body and brain.
How might sleep help or cause brain fog?!
Sleep is now believed to promote clearance from the brain of ‘metabolic waste’ that accumulates during the day, removing ‘molecular debris’ that affects proper brain function, such as neural signalling. This is via a system called the glymphatic system.
It was only discovered in 2012, and it is often compared to the lymphatic system, which is found throughout the body.
The glymphatic system is constantly filtering toxins from the brain, but during wakefulness, this system is largely turned off. During natural sleep, there is an expansion of the brain’s extracellular space, and this results in decreased resistance to fluid flow.
The increase in clearance happens specifically during non-rapid eye movement sleep. (source) For those that wear gadgets that allow you to monitor your sleep, you can consider whether you get healthy amounts of non-rapid eye movement sleep. If not, your glymphatic system won’t be working as much as it should be!
Interestingly and importantly, evidence has shown that other lifestyle choices, including sleep position, alcohol intake, exercise, omega-3 consumption, intermittent fasting, and chronic stress, all modulate the glymphatic clearance. (source)
This is wonderful to know and once again shows us the importance of improving our overall lifestyle.
Head Trauma
Brain fog is one symptom that has been underexplored in traumatic brain injury.
In one study, brain fog was higher in symptomatic mild traumatic brain injury and moderate-to-severe traumatic brain injury compared with healthy controls. Greater brain fog corresponded to greater depressive symptoms in symptomatic mild traumatic brain injury.
The authors concluded that brain fog appears to reflect challenges in recovery, including depressive symptoms and worse cognitive function. (source)
What’s going on here?
Traumatic brain injury involves two types of damage: primary and secondary. (source)
Primary damage refers to the brain damage produced by the trauma itself. It includes increases in intracranial pressure, haemorrhages, and edema, among others.
Secondary damage refers to the changes that occur hours to days after the head trauma, such as neuroinflammation, oxidative stress, and mitochondrial damage.
It is these secondary damage mechanisms that are responsible for the chronic symptoms, such as brain fog, but also increase vulnerability to new brain trauma or other neurodegenerative disorders such as Alzheimer’s.
(source)
So once again, we see neuroinflammation at the centre of things, and this is mainly due to glial cell activation. Remember that neuroinflammation (brain inflammation) is defined as “the innate immune response in the central nervous system to clear the system from damaged cells and infections”.
It is crucial for the regeneration of the central nervous system, but when neuroinflammation is chronic, it is detrimental to cells.
Early in TBI research, there has been evidence of neuroinflammation in the brain, such as proinflammatory cytokines production. (source)
The good news is that we have lots of ways to modulate inflammation, reduce oxidative stress, and support mitochondrial function (the three examples given of secondary damage).
How To Get Rid Of Brain Fog
Diet
A healthy, nutrient-dense diet ensures your brain is getting the nutrients it needs for optimal functioning. Including things like free-range eggs, olive oil, oily fish such as salmon and mackerel, and plenty of colour through in season and local fruit and vegetables.
You may like to consider removing some common food triggers, such as gluten, for a 30-day period. If you don’t notice any improvement, then bring it back in. Other common triggers include dairy and eggs.
Exercise
Exercise stimulates the production of a chemical called brain-derived neurotrophic factor, which helps promote repair and enhances the performance of connections between brain cells. Also, exercise pumps more blood up to the brain, ensuring it is getting the nutrients it requires to function at its best.
Optimise Your Circadian Rhythm
Nothing can work properly if our body clock is out of alignment. Some tips to help with this:
- Wake with the sun and get outside at sunrise.
- Limit exposure to blue light from sunset – wear blue light-blocking glasses and limit the use of technology in the evenings.
- Don’t drink caffeine after noon.
- Don’t use your phone in bed.
- Have an evening routine that acts as a cue to your mind and body that it’s time to start to wind down for the day. This could include a herbal tea, a bath, a stretch, a mindfulness practice, or reading a book.
- Limit alcohol use as much as possible.
- Try and have your bedroom pitch black, or buy an eye mask.
Cold Exposure
While this isn’t for everyone (not just because some people hate the idea of a cold shower, but because it can actually inhibit healing if your body can’t tolerate the stress caused by the cold exposure), it can have an immediate effect on some people brain fog due to it activating the vagus nerve and thus providing an anti-inflammatory benefit.
Supplements
The best supplements for you will depend on your unique situation – do you have a chronic gut issue? Thyroid issue? Mitochondrial issue? Or have you been exposed to mould and have a histamine issue?
Get 10% off supplements at healthpath with code ‘alexmanos10’.
Having said that, there are some key products to consider from a general perspective:
Luteolin
A liposomal luteolin formulation improved attention in children with ASDs and brain “fog” in mastocytosis patients (source)
Recommended Product: Luteolin.
Resveratrol
This study provides initial evidence that supplementary resveratrol improves memory performance in association with improved glucose metabolism and increased hippocampal functional connectivity in older adults. (source)
Recommended Product: Resveratrol
Omega 3 fatty acids
(source)
Recommended Product: Omega 3
Magnesium
(source)
Recommended Product: Magnesium.
B vitamins
(source)
Recommended Product; B Complex Plus
Probiotics
One study found that probiotics were associated with brain fog in those who had SIBO (source). As always context matters and this is not a reason to not try probiotics. Other research has actually found probiotics can improve cognition. This product unfortunately is only available when working with a practitioner.
Alex is a certified Functional Medicine Practitioner (IFMCP) and has a MSc in Personalised Nutrition. He is also a breathwork facilitator with a background in personal training and massage therapy. He also runs The Resiliency Program - a 24 week program aimed at building physical, mental, emotional, and spiritual resilience.