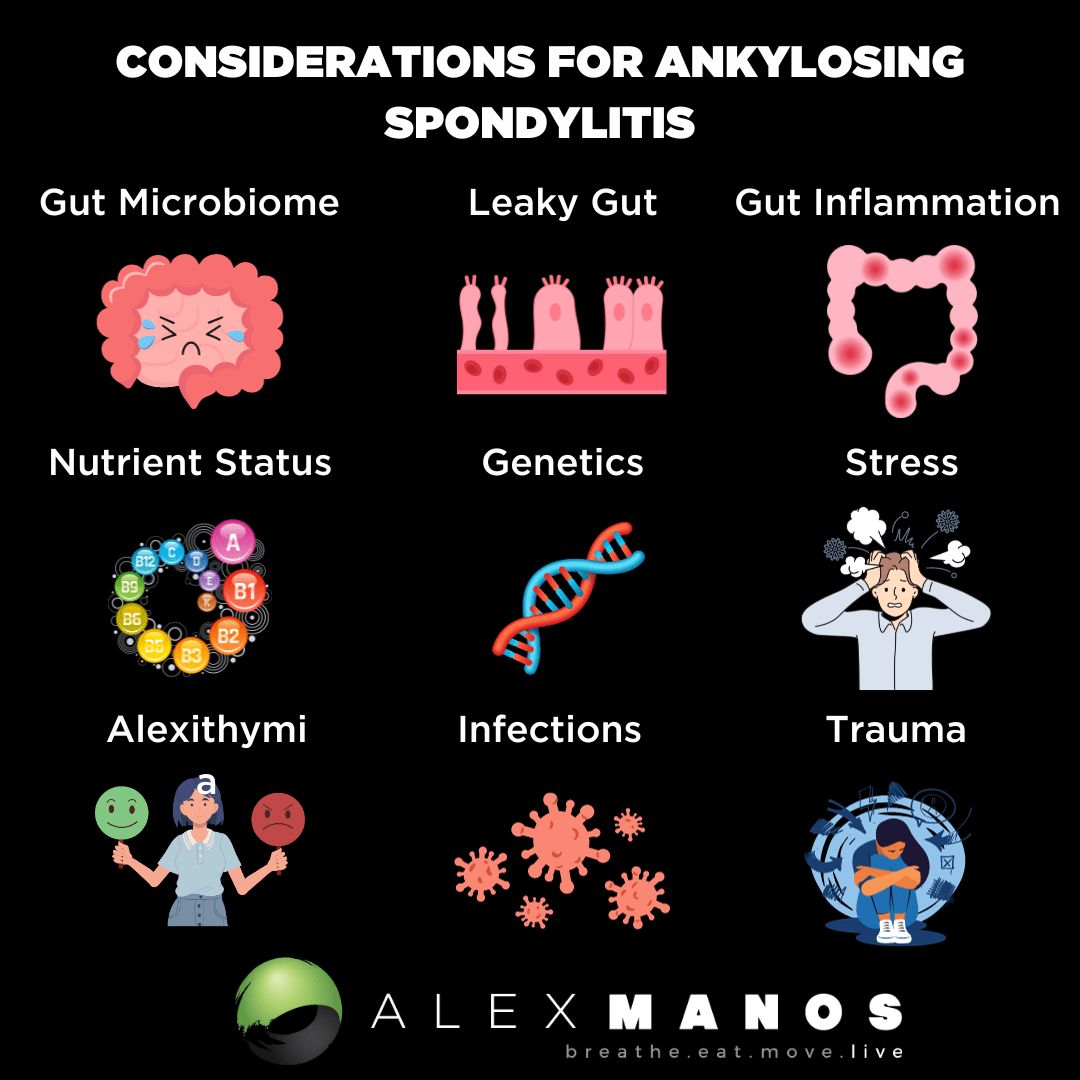
What Is Ankylosing Spondylitis?
Ankylosing spondylitis is a chronic inflammatory arthritis, thought by some to be autoimmune in origin.
It would appear that the most likely causative agent in the development of Ankylosing spondylitis is an environmental factor in the genetically susceptible, HLA-B27 positive, individuals.
What is HLA-B27?
It has been shown that more than 9 out of 10 people with Ankylosing spondylitis carry a particular gene known as human leukocyte antigen B27 (HLA-B27).
Having this gene doesn’t necessarily mean you’ll develop Ankylosing spondylitis. It’s estimated 8 in every 100 people in the general population have the HLA-B27 gene, but most don’t have Ankylosing spondylitis.
It’s thought having this gene may make you more vulnerable to developing Ankylosing spondylitis, but we need a trigger, or ‘causative agent’ – such as the bacteria klebsiella pneumoniae.
Associated Conditions
Its sphere may incorporate extra-articular features, including anterior uveitis and inflammatory bowel diseases (IBD) such as Crohn’s disease (CD) and ulcerative colitis (UC). The etiological mechanism of AS is complex, developing via the convergence of genetic, microbial, environmental, and immunological factors (source)
Klebsiella and Ankylosing spondylitis ?
One of the prime candidates for being an environmental factor, according to several reports, is the bacteria ‘Klebsiella pneumoniae’ which may trigger, or perpetuate, Ankylosing spondylitis:
Extensive data from several countries support the notion that Klebsiella pneumonia bacteria are the most likely culprit in the causation of Ankylosing spondylitis. These microbes possess antigens which resemble HLA-B27 and spinal collagens
This conclusion is based on evidence obtained from several disciplines:
- Immunogenetic studies show that there is molecular mimicry between HLA-B27 and Klebsiella
- Increased isolation of fecal Klebsiella has been reported in both Europe and North America
- Antibodies to Klebsiella have been demonstrated in ankylosing spondylitis patients in England and Finland
Research has also discussed the innate immune system with genome-wide analysis has also shown the association of several innate immune-related pathways and cytokines, which act as the effective therapeutic targets in Ankylosing spondylitis.
What Is The Mechanism Associateing Klebsiella Pneumoniae With Ankylosing Spondalytis?
Molecular mimicry, or, cross-reactivity hypothesis is suggested to be the main mechanism that can link Klebsiella with the initiation and development of Ankylosing spondylitis.
“Where a foreign antigen [such as a klebsiella] shares sequence or structural similarities with self-antigens”
Essentially what we are saying here is that klebsiella is so similar in structure to that of our own tissue, the immune system attacks the tissue thinking it is klebsiella.
The difference between other non-specific mechanisms that initiate autoimmunity and molecular mimicry is that microbial mimics specifically direct the immune response towards a tissue and/or organ. As mentioned in the above quote, klebsiella posses antigens which resemble spinal collagens – this is why back pain and stiffness are the most common symptoms.
The Gut Microbiome
The gut microbiome performs critical functions in the pathogenesis of Ankylosing spondylitis through various mechanisms, including:
- Interacting with genes.
- Enhancing intestinal permeability (aka leaky gut).
- Activating the gut mucosa immune system.
- Affecting the metabolites of our gut bacteria.
(source)
In the early stages of the disease, the diversity, structure, and function of the gut microbiota differ from healthy individuals. The microbiota dysbiosis affects the immune system locally and throughout the body, thus predisposing humans to several pathologies, including Ankylosing Spondylitis, IBD, reactive arthritis, etc.
Recent studies have shown that the occurrence and development of Ankylosing Spondylitis are related to changes in the diversity and composition of the gut microbiome. Let’s summarise some key findings:
- One studycfound that Bacteroides coprophilus, Parabacteroides distasonis, Eubacterium siraeum, Acidaminococcus fermentans, Prevotella copri were enriched in AS, while Enterococcus faecium E980 and TX0133a01 were reduced. (source)
- In a second study the researchers found that compared with HCs, relative abundance of Bacteroidetes was decreased in AS cases, but Firmicutes and Verrucobacterium were increased. Morever, specific gut bacteria were associated with disease activity of AS patients. (source)
- A third study found increased abundances of Lachnospiriaceae, Ruminococcus, Rikenellaceae, Porphyromonadaceae and Bacteroidaceae, but decreased abundance of Veillonellaceae and Prevotellaceae in the terminal ileum of AS patients. These findings suggest that some AS-rich species may be triggers of autoimmunity. (source)
- Research has found an increased abundance of specific Firmicutesspecies causes AS. The Firmicutes/Bacteroidetes (F/B) ratio has been widely associated with maintaining normal intestinal homeostasis. (source)
- And finally, researchers have observed changes in metabolites outside and inside the gut in AS patients (source)
Leaky Gut And Ankylosing Spondylitis
Increased permeability between intestinal epithelial cells results in the development of Ankylosing Spondylitis.
One group of researchers performed ileum biopsy in 50 patients with HLA-B27+ Ankylosing Spondylitis patients and 20 controls. They found invasive and adherent bacteria, mainly gram-negative bacteria such as Escherichia coli and Prevotella, were present in the ileum of Ankylosing Spondylitis patients, which was related to leaky gut.
Another study observed increased gut permeability in Ankylosing Spondylitis patients and their relatives.
Endotoxin-induced uveitis associated with Ankylosing Spondylitis in mice may provide evidence. Epithelial and endothelial leakage often gives zonulin and bacterial products the opportunity to enter the bloodstream, which may activate innate and adaptive immune responses.
However, there is still some debate in the research as to whether the loss of barrier integrity (leaky gut) is a cause or a consequence of imbalances in the gut microbiome.
Does Diet Help Ankylosing Spondylitis?
The main substrate that is necessary for the growth of the microbiome includes starch and complex carbohydrates which are usually available in considerable amounts in the large intestine (they are not 100% digested in the small intestine). Increased intake of high-starch diet is directly proportional to the gut-associated bacterial load, especially in the large intestine, and among these microbial agents, Klebsiella pneumoniae is considered as one of the main constituting components.
Therefore, increased starch consumption by genetically susceptible individuals, such as those possessing HLA-B27, could trigger the disease in Ankylosing spondylitis by enhancing the growth and perpetuation of the Klebsiella microbes in the bowel (3).
These results indicate that complex carbohydrates such as starch-containing products are necessary for the growth, replication, and persistence of many enterobacterial agents including Klebsiella microbes in the large bowel.
So it has been concluded that a low-starch diet intake alongside the currently used medical therapeutic modalities could be beneficial in the management of patients with early Ankylosing spondylitis.
It seems, therefore, that an exclusion of a diet containing complex carbohydrates such as starch, but not simple carbohydrate-containing foods such as glucose or sucrose, might inhibit the growth of Klebsiella and could ameliorate the disease process and activity in patients with AS.
There is also a well documented link between gut inflammation and Ankylosing spondylitis. Low starch diets may be helpful in lowering inflammation also.
To provide a balanced view on the research a systematic review published in 2018 on the role of diet in Ankylosing spondylitis concluded:
“Evidence on a possible relationship between Ankylosing spondylitis and diet is extremely limited and inconclusive due to the majority of included studies being small, single studies with moderate-to-high risk of bias, and insufficient reporting of results.”
I would argue against this conclusion, as many a client can testify! It seems clearly evident to me that there is a strong connection between the two that should be investigated in each client to see how they respond to both a low-starch diet, and/or treatment for supporting the microbiome and klebsiella pneumoniae.
In a study published in 2021 the authors concluded that patients with Ankylosing spondylitis should pay more attention to their diet to increase serum antioxidant status, as they found a lower intake of phytochemicals, and lower omega 3 fatty acid and vitamin C intake in patients with AS compared with controls (source).
Supplements To Consider:
- Saccharomyces Boulardii – a yeast strain of probiotic.
- Other probiotics of bacterial origin such as this example.
- Vitamin A and vitamin D – both essential for a healthy mucosal immune system (a part of the immune system that lines the gut)
- NAC which has anti-inflammatory, antioxifative and immune modulating properties
- Omega 3 fatty acids – these have shown to improve symptoms such as inflammation in those with inflammatory arthritic conditions.
Research
- https://www.ncbi.nlm.nih.gov/pubmed/29438717
- https://www.ncbi.nlm.nih.gov/pubmed/25385438
- https://www.ncbi.nlm.nih.gov/pubmed/23781254
- https://www.ncbi.nlm.nih.gov/pubmed/29657875
- https://www.ncbi.nlm.nih.gov/pubmed/1561397
- https://www.ncbi.nlm.nih.gov/pubmed/29852390
- https://www.ncbi.nlm.nih.gov/pubmed/29277308
- https://www.ncbi.nlm.nih.gov/pubmed/17062435
Alex is a certified Functional Medicine Practitioner (IFMCP) and has a MSc in Personalised Nutrition. He is also a breathwork facilitator with a background in personal training and massage therapy. He also runs The Resiliency Program - a 24 week program aimed at building physical, mental, emotional, and spiritual resilience.