Jump to the end of the blog for a summary of possible interventions if you know, or suspect, you have hydrogen sulfide SIBO. You may like to check out my section of my blog dedicated to gut health, click here.
Popular posts include:
- How To Treat SIBO Naturally: Probiotics
- How Do You Treat Hydrogen Sulfide SIBO?
- What Causes Hydrogen Sulfide SIBO?
- Methane: The Misunderstood Gas
What Is Hydrogen Sulfide?
Hydrogen sulfide is a colorless and odorless gas that is produced both by our own cells, and, by bacteria in the large intestine. Hydrogen sulfide has emerged as an important ‘gasotransmitter’ that regulates several bodily systems including: the cardiovascular, digestive, immune, hormonal, and nervous systems.
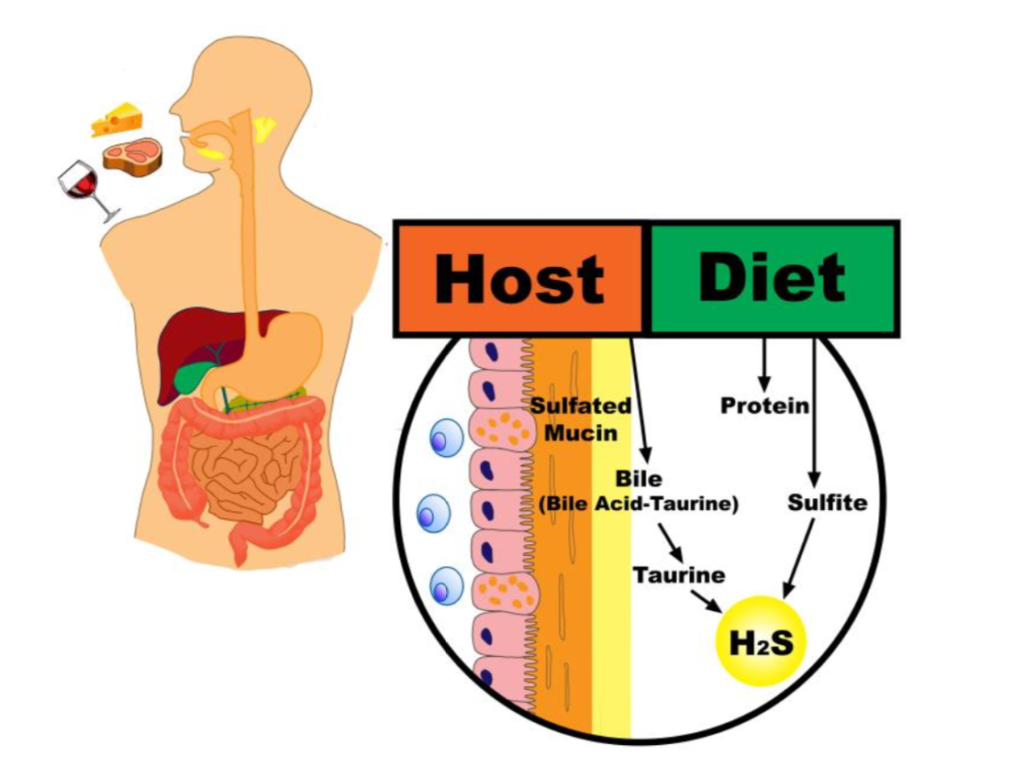
Teigen et al., Nutrients 2019, 11, 931
What Is Hydrogen Sulfide SIBO?
Hydrogen sulfide SIBO is the term used when someone has an overgrowth of sulphate reducing bacteria in their intestines. It is not currently tested for in the hydrogen SIBO breath test. However, when both hydrogen and methane gasses come back extremely low throughout the three hours, it is thought this may indicate hydrogen sulfide is being excessively produced.
Here is a SIBO example report from Healthpath:
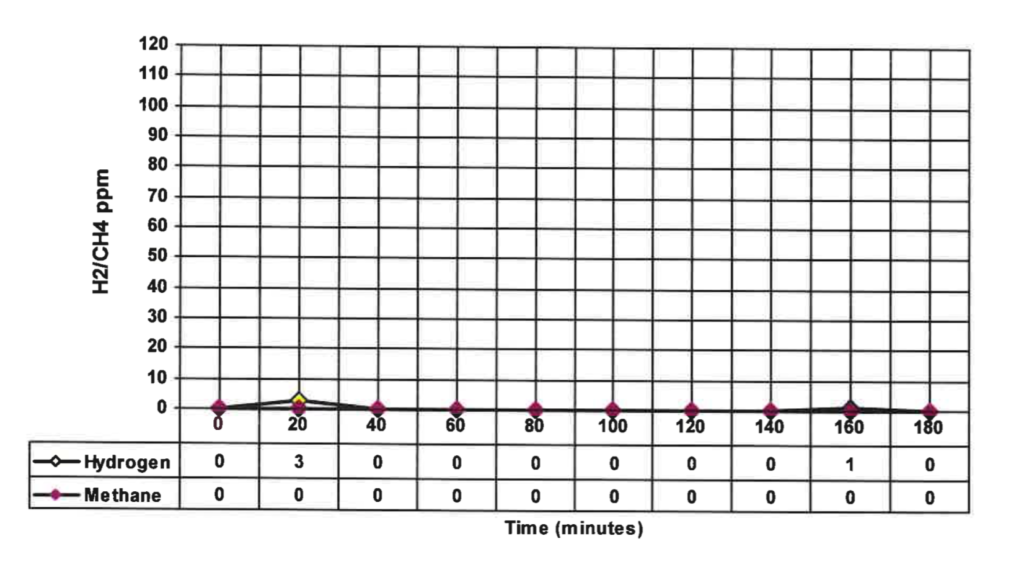
We expect to see a rise in hydrogen gas from approximately the 90 minute mark onwards. When this doesn’t occur, and methane levels are also very low, we can start to consider hydrogen sulfide, is being excessively produced. To help understand whether this is the case, assessing the microbiome via stool testing to evaluate the levels of hydrogen sulfide producing bacteria may be helpful (more on this below).
How Is Hydrogen Sulfide Produced In The Body?
The precise locations of its production remain an active area of research.
Hydrogen sulfide is produced endogenously through several enzymes, including:
- Cystathionine β-lyase (CBE)
- Cystathionine γ-lyase (CSE)
- 3-mercaptopyruvate sulfurtransferase (MST)/cysteine aminotransferase (CAT)
These specific enzymes are expressed accordingly in various organ systems.
From what I understand thus far, based on Dr. Nigh’s theory, when healthy cells are put under stress, such as hypoxic conditions, a hydrogen sulfide-producing enzyme called cystathionine-gamma-lyase (CSE) moves from the cytosol (inside) of the cell, to the outer mitochondrial membrane, where it uses cysteine, an amino acid, to generate Hs2. The hydrogen sulfide produced actually supports energy production. Dr. Nigh puts it well by stating:
The point is that Hs2 production is vital to the cellular adaptation to physiological stress.
However hydrogen sulfide is also produced by gut bacteria and this is the main topic of today’s post.
The bacteria that reside in our digestive tract aid in the breakdown of nutrients from our food. Certain bacteria break down complex carbohydrates (like dietary fibre) into short-chain fatty acids (e.g butyrate), and gases (e.g., hydrogen) that are released or absorbed by the body.
Organisms called ‘hydrogenotrophs’ (essentially hydrogen consuming bacteria and archaea – click here for my blog on methane SIBO), are essential in keeping gut hydrogen levels low and stabilising the environment. Among the groups of hydrogenotrophs are methanogens (producing methane), acetogens (producing acetate), and sulfate reducing bacteria (producing hydrogen sulfide).
The methanogenesis/sulfate reduction ratio is dependent on substrate availability, thermodynamics and pH. In human colon, the ratio is in the favor of methanogenesis, due to neutral pH of stool and low sulfate levels in diet. However, in certain conditions, such as high availability of sulfate substrates in a diet (bread, beer, wine) and hypochlorhydria, sulfate reduction may become the major process
To break this down: bacteria ferment some of our food producing hydrogen gas. Certain types of bugs (methanogens and sulfate reducing bacteria mainly) compete for the hydrogen and use it to produce methane and hydrogen sulfide respectively. We utilise or expelle these gases by our breath and flatulence.
Watch my interview with Dr. Siebecker on hydrogen sulfide SIBO and prokinetics:
Sulfate Reducing Bacteria
The primary hydrogen sulfide producing bacteria include:
- Bilophila wadsworthii
- Desulfomonas pigra
- Desulfovibrio piger
It is thought that the microorganisms have quite a substantial role to play in hydrogen sulfide production based on animal studies demonstrating that:
Microbial produced hydrogen suldife is a significant contributor to the bodies hydrogen sulfide pool, as germ free mice have between 50 and 80% less hydrogen sulfide in their tissues and circulation.
We can evaluate our levels of Hs2 producing bacteria via stool testing available at Healthpath.

The following quotes summarise the systems and processes hydrogen sulfide may influence and how it may influence them:
H2s And Glucose Homeostasis
H2S has emerged as an important regulator of glucose homeostasis [blood sugar control]. This is achieved through its production and action in several metabolic and hormone producing organs including the pancreas, liver, and adipose.
Hydrogen Sulfide And Cardiovascular Health
Gut bacteria-derived metabolites may cross the gut-blood barrier and target blood vessels, the heart and other organs involved in the regulation of the circulatory system. A number of studies have shown that hydrogen sulfide is an important biological mediator in the circulatory system.
In short, H2S is synthetised in various tissues involved in circulatory system homeostasis, including the heart, blood vessels, kidneys and the brain
Changes in colonic hydrogen sulfide homeostasis may be associated with hypertension.
Hydrogen Sulfide And Digestive Health
H2S can damage the gastrointestinal epithelium (cause leaky gut)
Those with constipation-predominant IBS have been found in some studies to have a bacterial imbalance, in particular, a significant increase of sulfate reducing bacteria, and fecal sulfide, indicating a potential role for sulfide in the development of IBS symptoms.
From clinical studies with human volunteers and experimental works with rodents, it appears that hydrogen sulfide can exert mostly pro- but also anti-inflammatory effects on the colonic mucosa [gut lining].
Increased detection of Fusobacterium (a species of bacteria) in colorectal cancer tumors has been reported in two independent studies. Fusobacterium produce Hs2 through cysteine desulfhydrase activity – a hydrogen sulfide-producing enzyme. As hydrogen sulfide has been demonstrated to be genotoxic, the authors of this paper hypothesised that it may be one causative metabolite in the etiology of colorectal cancer.
Recently, a culture-dependent study demonstrated that mucosal biopsies from IBD patients were more often colonized by Fusobacterium spp. than those from matched healthy controls.
A key point here for us folk who are regularly interpreting stool tests is that fusobacteriam species may produce Hs2 gas via different mechanisms to that of those mentioned above (Bilophila wadsworthii, Desulfomonas pigra, Desulfovibrio piger).
Diet And Hydrogen Sulfide
Magee and colleagues demonstrated that dietary protein intake positively correlates with fecal sulfide concentrations in healthy individuals
The sulfur content of food can be estimated using the sulfur-containing amino acids (methionine and cysteine) as surrogates, but this fails to account for sulfur-containing food modifiers or additives, such as sulfiting agents often found in processed food such as a bacon, sausages and other products (e.g., potassium bisulfate, sodium bisulfate), sulfuric acid, or carrageenan.
Dietary input and small intestinal absorption are considered the main determinants of sulfur delivery to the colon. The small intestine has an efficient but saturable dietary sulfate absorptive capacity of ~5–7 mmol/day. Once dietary sulfate intake exceeds ~5–7 mmol/day the amount reaching the colon increases linearly with intake.
Therefore, the amount of dietary sulfur that reaches the colon, particularly with increasing levels, can be generally assumed to parallel dietary intake.
A number of additional factors, however, such as food preparation (e.g., cooked versus uncooked, cooking temperature and method, ground versus whole), meal consumption habits (e.g., chewing), and transit time have been shown to influence small intestinal absorption of sulfur-containing molecules and the total amount of sulfur reaching the colon
Not all research aligns however. A paper published this year that looked at short-term changes in dietary sulfur on the relative abundances of intestinal sulfate-reducing bacteria concluded:
These results suggest that the use of dietary interventions alone may be insufficient for rapid therapeutic targeting of sulfate-reducing bacteria.
It should be noted that this study used 10-14 day periods, not very long!
Fibre And Hydrogen Sulfide
Although brassica vegetables are technically considered to be high sulfate foods, they also have a high fiber content. These findings underscore the beneficial role for the latter within the hydrogen sulfide toxin hypothesis and support a clinical approach focusing on plant versus animal-based diets rather than high- and low-sulfur diets.
Production of hydrogen sulfide …. is effectively suppressed by readily fermentable fibers.
The addition of FOS [a prebiotic] to slurries containing cysteine significantly suppressed Hs2
A good FOS supplement can be found here.
Cysteine And Hs2 Production
We have already mentioned the species of bacteria Fusobacterium that can produce hydrogen sulfide via the amino acid cysteine. Other bacteria that can convert cysteine to hydrogen sulfide include:
Several anaerobic bacterial strains (Escherichia coli, Salmonella enterica, Clostridia and Enterobacter aerogenes)
A recent in vitro study that profiled gas production from incubated fecal samples implicated cysteine specifically as a primary driver of H2S production—conversely, the effect of sulfate was small. Cysteine degradation to H2S is catalyzed by enzymes with cysteine desulfhydrase activity
In fact, in vitro modeling using healthy human feces suggests that the contribution of cysteine to H2S production is substantially more than that from sulfate
Escherichia coli possess several enzymes with cysteine desulfhydrase activity
In addition, gut bacteria may produce H2S by sulfite reduction. Sulfite reductase is present in many species such as E. coli, Salmonella, Enterobacter, Klebsiella, Bacillus, Staphylococcus, Corynebacterium, and Rhodococcus
The Importance Of The Liver & Detoxification of H2S
Systemic effects of colon-derived H2S and/or its derivatives may be in part due to some liver-dependent mechanisms
Genetics And Hydrogen Sulfide
Given that most of the colonic disorders for which a potential pathogenic role for sulfide exists are effectively gene-environment disorders, it is straight-forward to envision how common polymorphisms in host genes encoding components of the sulfide oxidation pathway might underlie ineffective epithelial sulfide detoxification and thereby predispose certain individuals to chronic sulfide-generated inflammation or genotoxicity.
Dr. Nigh in his article in NDNR (link at end of this blog under resources) mentions:
Genetics comes into play in this as well, though my clinical experience suggests that outside of polymorphisms in the SUOX gene, the polymorphisms associated with cystathionine-beta-synthase (CBS) and CSE are usually playing a relatively minor role in sulfate production and processing.
These can be tested for via Lifecode GX – I had Emma from Lifecode GX on the podcast (episode 30) for those interested – a fountain of knowledge on this topic.
Hydrogen Sulfide Symptoms
- Hives
- Halitosis
- Hot flashes
- Chronic fatigue syndrome
- Dermatitis
- Brain fog
- Inflammatory bowel disorders
- Hypertension
- Atherosclerosis
- Heart failure
- Diabetes
- Cirrhosis
- Inflammation
- Sepsis
- Neurodegenerative disease
- Erectile dysfunction
- Asthma
- ….to name a few.
Anecdotally ‘rotten egg’ smelling flatulence has been associated with hydrogen sulphide SIBO.
Testing For Hydrogen Sulfide
There is not a current validated test for Hs2 in the U.K (there is in the U.S). However you can test for levels of sulphate reducing bacteria via stool testing, and thus gain good understanding around whether there is a microbial imbalance contributing to Hs2 imbalances.
Also a ‘flat lining’ SIBO breath test may indicate an overgrowth of hydrogen sulphide bacteria, and thus, breath testing for SIBO may provide additional information. But remember, we now know that a flat lining SIBO set of results is not 100% accurate and you can have hydrogen and hydrogen sulfide production.
Click here to see the bacteria, yeasts, parasites, worms, and functional markers we test for.
How Do You Reduce Hydrogen Sulfide?
high colonic H2S levels may be responsible for colonic inflammation and cancer. On the other hand, recent studies suggest that colonic epithelial cells are well-adapted to the H2S-rich environment, and that H2S plays a beneficial role in the protection of the GBB [gut blood barrier]
Microbial H2S has been associated with both maintaining gastric health and being implicated in disease. Several groups have shown that H2S regulates various physiological functions including maintenance of GI barrier function and injury repair
As these quotes demonstrate there is still a lot that we need to learn, and, what to do is very much context dependent. It seems considerations may include:
- Molybdenum can be a real game changer, especially if struggling with diarrhoea.
- Whether we have a genetic predisposition meaning we may need to be more mindful of sulfur requirements and thus intake. I love Lifecode GX who, via practitioners, offer excellent clinically relevant testing here. It was game changing in my own health journey and really helps you understand why you might be having the issues you’re having. Watch my podcast with founder Emma Beswick below where we talk about histamine and genetics.
- Testing to investigate the underlying causes of our symptoms further.
- A plant based, high fibre diet may be helpful, to what ever degree is tolerated.
- Turmeric might be helpful too.
- Considering toxin exposure which may increase our requirements for sulfur. For example some mycotoxins, that we might be breathing in if we live in a mould, damp, water-damaged building effect sulfur metabolism.
- Dr. Nigh recommends epsom salt baths, hydroxycobalamin (vitamin B12), Korean ginseng.
- Dr. Nigh also recommends a specific low-sulfur diet that is customised to each patient. In some circumstances we may need to lower our intake, while we seek to restore some health, integrity, balance to the microbiome and gut, before we then re-diversify.
- Bismuth subsalicylate (sold under the brand name Pepto-Bismol) has been shown to dramatically reduce Hs2
- Supporting digestion via digestive enzymes and stomach acidity.
Dr. Ruscio has a useful and interesting low sulfur diet handout that can be found by clicking here.
I would like to add this article is for educational purposes only – if you know or suspect you have imbalances in the microbiome, or Hs2 production/clearance then I highly recommend working with an experienced practitioner to support you through the process of understanding your underlying imbalances and strategies required to restore health.
All in all there is a lot for us to consider and this quote seems apt. to finish with:
The metabolic milieu in the lumen of the colon, however, is the result of a multitude of factors beyond dietary sulfur intake and sulfate-reducing bacteria abundance.
Resources
There is an interesting case study by Dr. Nirola Jacobi you may like to read: click here.
There is also an interesting article on it being an adaptive response: click here.
References
- Jennifer Pichette and Jeffrey Gagnon (2016) Implications of Hydrogen Sulfide in Glucose Regulation: How H2S Can Alter Glucose Homeostasis through Metabolic Hormones: click here
- Tomasova et al., (2016) Gut Bacteria and HS2: The New Old Players in Circulatory System Homeostasis: click here.
- Teigan et al., (2019) Dietary Factors in Sulfur Metabolism and Pathogenesis of Ulcerative Colitis: click here
- Carbinero et al., (2012) Microbial pathways in colonic sulfur metabolism and links with health and disease: click here.
- Wallace et al., (2018) Hs2: an agent of stability at the microbiome-mucosa interface: click here.
- Wang R. Physiological implications of H2S: a whiff exploration that blossomed: click here
- Fu M, Zhang W, Wu L, et al.H2S metabolism in mitochondria and its regulatory role in energy production: click here.
- Yao et al., (2018) Modulation of colonic hydrogen sulfide production by diet and mesalazine utilizing a novel gas-profiling technology
- Suarez et al., (1998) Bismuth subsalicylate markedly decreases Hs2 release in the human colon: click here.
- Webster et al., (2019) Influence of short-term changes in dietary sulfur on the relative abundances of intestinal sulfate-reducing bacteria: click here.
- Sing & Lin, (2015) Hs2 in Physiology and Diseases of the Digestive Tract: click here.
- Linden, (2014) HS2 Signaling in the Gastrointestinal Tract: click here
- Huang et al., (2015) A cardioprotective insight of the cystathionine γ-lyase/hydrogen sulfide pathway: click here
Alex is a certified Functional Medicine Practitioner (IFMCP) and has a MSc in Personalised Nutrition. He is also a breathwork facilitator with a background in personal training and massage therapy. He also runs The Resiliency Program - a 24 week program aimed at building physical, mental, emotional, and spiritual resilience.