Depression is becoming an increasingly common condition. There are a multitude of factors as to why someone may develop depression from traumatic events in their childhood (referred to as ACE’s, or, adverse childhood advents in the research), or feelings of loneliness, or a lack of purpose or meaning in life, to nutrient deficiencies, imbalances in digestive health, and hormone imbalances. We could go on here.
The purpose of today’s blog is to focus on the role that our gut health may play in depression.
Research has demonstrated that imbalances in the gut can contribute to mood based conditions such as depression.
The gut microbiome has been discussed in the research as a “regulator of depression”. Interestingly there is a growing consensus that Inflammatory Bowel Disease (a gut based autoimmune condition) is associated with anxiety- and depression-related symptoms, and, these psychological symptoms appear to be more prevalent during active disease states. This indicates that imbalances in gut health directly influence mental well-being.
Depression: The Gut Brain Axis
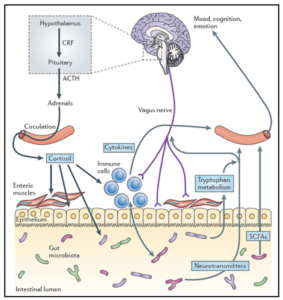
One of the ways our gut health can influence our mental wellbeing is via the gut brain axis. The gut brain axis is made up of several ‘communication pathways’ between the gut and the brain. These include:
- An immune pathway
- A hormone pathway
- A metabolite pathway
- A neurological pathway
In the most simplistic terms these pathways, which we refer to as the gut brain axis, are what interconnect these two areas of the body and partly explain why psychological stress can cause symptoms such as butterflies in the stomach, bloating, diarrhoea, constipation and abdominal pain, and, why imbalances in our gut health might contribute to mood based disordered such as depression.
- The neurological pathway is made up the vagus nerve. Vagus in latin means ‘wandering’ so you can invision what this nerve looks like – branching out from the base of the brain and connecting all our vital organs in the torso.
- The immune pathway is made up, partly, of cytokines – these are immune cells involved in the inflammatory response.
- The hormone pathway includes hormones such as cortisol – the stress hormone.
- The metabolite pathway includes short chain fatty acids – these are produced by bacteria in our large intestine fermenting our dietary fibre. These SCFA’s, an example being butyrate, can travel across the gut wall, into circulation and in to the nervous system.
Depression and Medications
Recurrent antibiotic exposure is associated with increased risk for depression and anxiety
Another layer of evidence that gut health directly influences our mood is that there is an association between antibiotic usage and our risk of depression.
Proton Pump Inhibitors may also contribute to depression among other conditions:
There is a direct association between the onset of dementia and depression on one side and the long-term use of PPIs on the other.
Depression: Nutrition
There is research discussing the role of specific nutrients in depression too.
These include zinc, selenium, magnesium, B vitamins including vitamin B12, B6 and folate, and vitamin D. A test called The Optimal Nutrient Evaluation, offered by Genova Diagnostics, is a great at-home urine test to evaluate many of these nutrients.
Meta-analyses support the adjunctive use of zinc in major depression.
Depression: Diet
There is no specific diet to optimise the axis however supporting overall gut health may be helpful. Some of the most important considerations then include:
- Eating a wide range of plant foods. I recommend a daily goal, and a weekly goal here:
- The saying is eat a rainbow a day and thus ensuring you eat at last one portion of food from each of the colour groups may be important.
- Aim for 30+ different plant foods per week (vegetable, fruit, herbs, spices, nuts, seeds, pulses, lentils, legumes, beans, whole grains).
- Eat adequate amounts of healthy fats – aim to eat oily fish three times per week, avocados, nut, seeds, eggs, olive oil, ghee, grass fed dairy if tolerated.
- Eat fermented foods regularly – kombucha, kefir, kimchi and sauerkraut are the most popular options.
These are all bottom-up considerations (things that support gut health which may influence brain health). But don’t forget the important role that sleep, exercise and managing stress also play on both brain health and gut health. As always we need to focus on a lifestyle, not just a diet.
Depression: Supplements
Things to consider to support gut health include:
- Probiotics: some strains of probiotic are termed psycobiotics as they have shown in studies to influence mood and behaviour. An example of this is L. plantarum 299v. This is found in the supplement Ideal Bowel Support by Jarrow: click here. Receive 10% off by using my name (Alex Manos) during check out.
- Omega 3: these healthy anti-inflammatory fats have been shown to increase butyrate producing bacteria and are helpful for brain health. Remember we mention butyrate earlier as a short chain fatty acid which make up part of the gut-brain axis. There is a product by APEX called ‘Brain E DHA 1200-TG (K114)’ which is an excellent option. It is available via Amrita but you will need to register to be able to order it: click here.
- Prebiotics: I like Bimuno available from Amazon (click here). I add this to my morning coffee for a gut-friendly start to the day!
- Vitamin D may have exert some of its positive influence via the gut-brain axis.
Summary
I am increasingly a man of simplicity. So general considerations to improve the axis include:
- A paleo-mediterranean style diet – to be used as a framework.
- Adequate sleep – which needs to include deep sleep – the most restorative kind.
- Daily activity.
- Managing our stress levels: This may include incorporating some meditation, tai chi, yoga, breathwork in to our daily routine. Please do not ignore or underestimate what for many is the most important intervention.
- The cultivation of a healthy emotional state and mindset – practicing gratitude and learning tools from positive psychology.
More personalised recommendations may be considered in the context of an individuals health, lifestyle, health history and functional testing. For example results from a microbiome stool test.
I would like to finish by reiterating the importance of purpose and meaning in life. The importance of movement and exercise (at what ever level you are capable of). And the importance of connection, relationships and expressing ourselves through some avenue – this could be art, music, journalling, singing, dancing (even if just on your own in your living room to your favourite music).
Also, don’t let perfection get in the way of progress. 1 minute of movement, a little dancing to some music – it does help, but not necessarily immediately. They need to be done consistently, over a extended period of time. Patience and trusting the process are huge when it comes to recovering from chronic complex health issues. I think this is why having a coach supporting you through your journey can be so valuable. Some one who has guided many people through this journey and as a result has wisdom and experience they can share with you along the road.
Resources
A great book on probiotics and gut health in mood based disorders is called The Psychobiotic Revolution.
A more comprehensive look at depression is a book called Lost Connection by Johann Hard: click here.
References
- Zinc, Magnesium, Selenium and Depression: A Review of the Evidence, Potential Mechanisms and Implications.
- The Emerging Role for Zinc in Depression and Psychosis: click here.
- The effects of probiotics on depressive symptoms in humans: a systematic review: click here.